The vestibulocochlear nerve, also known as the eighth cranial nerve, plays a crucial role in our ability to hear and maintain balance. It is essential to understand the anatomy, function, and various disorders associated with this nerve. In this article, we will explore the pathway of the vestibulocochlear nerve through the cranium, its relationship with surrounding structures, medical imaging techniques used for diagnosis, and treatment options for vestibulocochlear nerve disorders.
Understanding the Vestibulocochlear Nerve
The vestibulocochlear nerve, also known as the eighth cranial nerve, is a crucial component of our sensory system. It plays a vital role in our ability to hear and maintain balance. Let’s delve deeper into the anatomy and function of this fascinating nerve.
Anatomy of the Vestibulocochlear Nerve
The vestibulocochlear nerve consists of two main branches: the cochlear branch and the vestibular branch. These branches work in harmony to ensure our auditory and vestibular systems function properly.
The cochlear branch, as the name suggests, is primarily responsible for auditory function. It originates from the cochlea, a spiral-shaped structure within the inner ear that is crucial for hearing. This branch carries auditory information from the cochlea to the brain, allowing us to perceive and interpret sound.
On the other hand, the vestibular branch is responsible for our sense of balance and spatial orientation. It arises from the vestibular apparatus, a complex system of fluid-filled canals and sensory organs located within the inner ear. The vestibular branch carries signals related to balance and spatial orientation from the vestibular apparatus to the brainstem.
Both the cochlear and vestibular branches of the vestibulocochlear nerve unite to form a single nerve before entering the cranium. This union ensures efficient transmission of sensory information to the brain, enabling us to make sense of the world around us.
Function of the Vestibulocochlear Nerve
The vestibulocochlear nerve is a sensory nerve that plays a crucial role in our ability to perceive sound and maintain balance. Let’s explore the functions of its two main branches in more detail.
The cochlear branch of the vestibulocochlear nerve is responsible for transmitting auditory information from the cochlea to the brain. The cochlea acts as a transducer, converting sound vibrations into electrical signals that can be interpreted by the brain. This branch carries these signals, allowing us to hear and distinguish different sounds, ranging from the softest whisper to the most thunderous roar.
On the other hand, the vestibular branch of the vestibulocochlear nerve is involved in our sense of balance and spatial orientation. The vestibular apparatus, which includes the semicircular canals and otolith organs, detects changes in head position and movement. The vestibular branch carries these signals to the brainstem, where they are processed and integrated with visual and proprioceptive information to maintain our balance and coordinate our movements.
Without the vestibulocochlear nerve, our ability to hear and maintain balance would be severely compromised. It is truly remarkable how this intricate network of nerves and sensory organs work together to provide us with such essential functions.
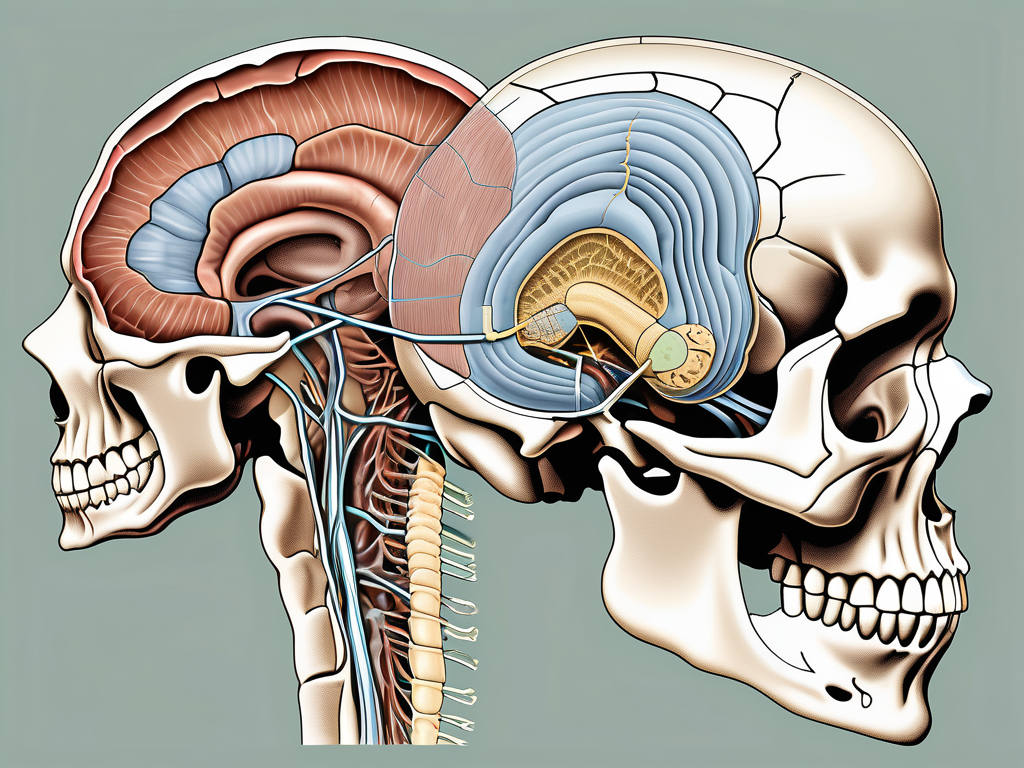
The Path of the Vestibulocochlear Nerve through the Cranium
Origin and Course of the Vestibulocochlear Nerve
The vestibulocochlear nerve, also known as the eighth cranial nerve, is a crucial component of the auditory and vestibular systems. It originates from the inner ear, specifically the cochlea and vestibular apparatus, which play essential roles in hearing and balance.
As the vestibulocochlear nerve begins its journey, it navigates through the intricate structures of the temporal bone. This bone, located on the sides of the skull, houses and protects the delicate inner ear structures. Within the temporal bone, the nerve passes through a narrow canal known as the internal auditory meatus.
The internal auditory meatus, situated in the petrous portion of the temporal bone, serves as a protective conduit for the vestibulocochlear nerve. This bony canal not only shields the nerve but also provides a pathway for it to travel from the inner ear to the cranial cavity.
The Vestibulocochlear Nerve and the Internal Acoustic Meatus
The internal acoustic meatus, a fascinating anatomical feature, is a narrow passageway within the temporal bone. Alongside the vestibulocochlear nerve, it accommodates other vital structures, including the facial nerve, also known as the seventh cranial nerve.
Within the internal acoustic meatus, the vestibulocochlear nerve and the facial nerve are in close proximity. This proximity can sometimes lead to clinical implications, as any pathology affecting one nerve may potentially impact the other. For example, certain tumors or infections within the internal acoustic meatus can affect both the vestibulocochlear and facial nerves, leading to symptoms such as hearing loss and facial weakness.
Understanding the intricate path of the vestibulocochlear nerve through the cranium is crucial for medical professionals involved in diagnosing and treating conditions related to hearing and balance. By comprehending the complex anatomy of the inner ear and its surrounding structures, healthcare providers can better assess and manage patients with vestibulocochlear nerve disorders.
The Relationship between the Vestibulocochlear Nerve and Surrounding Structures
The vestibulocochlear nerve, also known as the eighth cranial nerve, plays a vital role in our ability to hear and maintain balance. It is responsible for transmitting auditory and vestibular information from the inner ear to the brain. Let’s explore the intricate relationship between the vestibulocochlear nerve and its surrounding structures in more detail.
The Vestibulocochlear Nerve and the Facial Nerve
Within the internal acoustic meatus, a narrow bony canal located in the temporal bone, the vestibulocochlear nerve and the facial nerve run adjacent to each other. This close proximity can have significant implications when it comes to certain pathologies.
Occasionally, tumors or other abnormalities can affect both the vestibulocochlear nerve and the facial nerve simultaneously. This can lead to a variety of symptoms, including auditory disturbances such as hearing loss or tinnitus, as well as facial weakness or paralysis. Prompt diagnosis and management of these conditions are crucial to minimize potential complications and preserve the patient’s quality of life.
The Vestibulocochlear Nerve and the Brainstem
Once the vestibulocochlear nerve enters the cranial cavity through the internal acoustic meatus, it connects with the brainstem. The brainstem, located at the base of the brain, is a crucial structure involved in various vital functions, including the processing and interpretation of sensory information.
Integration with the brainstem allows the vestibulocochlear nerve to transmit auditory and vestibular signals to the appropriate areas of the brain for further processing. This intricate network of connections enables us to perceive sound and maintain balance, two essential aspects of our daily lives.
When the vestibulocochlear nerve is functioning optimally, it ensures that the auditory information we receive is accurately relayed to the brain, allowing us to appreciate the richness and complexity of the sounds around us. Additionally, it helps us maintain a stable sense of balance, preventing falls and facilitating smooth movements.
However, when the vestibulocochlear nerve is compromised due to injury, infection, or other factors, it can result in a range of symptoms. These may include hearing loss, dizziness, vertigo, problems with coordination, and difficulties with spatial orientation.
Understanding the relationship between the vestibulocochlear nerve and the surrounding structures is crucial in diagnosing and managing conditions that affect its function. By recognizing the intricate connections and dependencies, healthcare professionals can provide appropriate interventions to restore or improve the patient’s auditory and vestibular capabilities.
In conclusion, the vestibulocochlear nerve is a remarkable structure that plays a fundamental role in our ability to hear and maintain balance. Its relationship with the facial nerve and the brainstem highlights the complexity of the human nervous system and the importance of its proper functioning for our overall well-being.
Disorders Related to the Vestibulocochlear Nerve
Vestibular Schwannoma
Vestibular schwannoma, also known as acoustic neuroma, is a benign tumor that usually develops from the vestibular branch of the vestibulocochlear nerve. This tumor grows slowly and can cause hearing loss, tinnitus, dizziness, and imbalance. Medical intervention is necessary to manage these cases, and treatment options depend on the tumor’s size, location, and the patient’s overall health.
When a vestibular schwannoma develops, it typically arises from the Schwann cells that surround the vestibular branch of the vestibulocochlear nerve. These cells, which are responsible for providing support and insulation to nerve fibers, start to multiply uncontrollably, forming a tumor. As the tumor grows, it can exert pressure on the surrounding structures, including the cochlear nerve, leading to hearing loss and other related symptoms.
Diagnosing a vestibular schwannoma often involves a combination of medical history review, physical examination, and diagnostic tests. Magnetic resonance imaging (MRI) is commonly used to visualize the tumor and determine its size and location. Additionally, audiometric tests may be performed to assess the extent of hearing loss and evaluate the patient’s overall auditory function.
Vestibulocochlear Nerve Damage and Hearing Loss
Injuries or damage to the vestibulocochlear nerve can result in hearing loss, as well as problems with balance and spatial orientation. Causes of nerve damage may include trauma, infections, exposure to loud noise, or certain medical conditions. It is crucial to seek medical attention and undergo appropriate diagnostic tests to determine the underlying cause and explore suitable treatment options.
When the vestibulocochlear nerve is damaged, the transmission of sound signals from the inner ear to the brain is disrupted. This disruption can lead to a range of hearing impairments, varying from mild to profound. In addition to hearing loss, individuals may experience difficulties with balance and coordination due to the nerve’s role in maintaining equilibrium.
Various factors can contribute to vestibulocochlear nerve damage. Traumatic injuries, such as head trauma or skull fractures, can directly affect the nerve’s integrity. Infections, such as meningitis or otitis media, can also lead to nerve damage if left untreated. Prolonged exposure to loud noises, such as in occupational settings or during recreational activities, can gradually damage the nerve fibers, resulting in hearing loss over time.
When seeking medical attention for vestibulocochlear nerve damage, healthcare professionals will conduct a thorough evaluation to determine the cause and extent of the injury. This evaluation may involve a combination of physical examinations, hearing tests, imaging studies, and other specialized tests to assess the nerve’s function. Once the underlying cause is identified, appropriate treatment options can be explored, which may include medication, surgery, or the use of hearing aids or cochlear implants.
Medical Imaging of the Vestibulocochlear Nerve
MRI Scans and the Vestibulocochlear Nerve
Magnetic resonance imaging (MRI) scans provide detailed images of the brain and its structures, including the vestibulocochlear nerve. This non-invasive imaging technique utilizes a strong magnetic field and radio waves to generate cross-sectional images of the body. MRI scans play a vital role in diagnosing vestibulocochlear nerve disorders, such as vestibular schwannomas.
When it comes to evaluating the vestibulocochlear nerve, MRI scans offer several advantages. Firstly, they can assess the size, location, and characteristics of vestibular schwannomas, which are benign tumors that can develop on the nerve. By accurately visualizing these tumors, healthcare professionals can determine the appropriate treatment plan, whether it involves surgical removal, radiation therapy, or monitoring for any changes over time.
Moreover, MRI scans can also help identify other abnormalities or conditions that may affect the vestibulocochlear nerve. For example, they can detect inflammation or infection in the surrounding structures, such as the inner ear or the brainstem. This information is crucial in determining the underlying cause of symptoms like hearing loss, dizziness, or balance problems.
CT Scans and the Vestibulocochlear Nerve
Computed tomography (CT) scans are another imaging modality commonly used to evaluate the bony structures surrounding the vestibulocochlear nerve. Unlike MRI, CT scans utilize X-rays to create detailed cross-sectional images of the body. They are particularly useful in assessing the temporal bone, which houses the inner ear structures and the vestibulocochlear nerve.
CT scans provide valuable information about the integrity of the bony structures that protect the vestibulocochlear nerve. They can detect fractures, deformities, or other abnormalities that may impact the nerve’s function. For instance, a temporal bone fracture resulting from trauma can lead to damage or compression of the nerve, causing symptoms like hearing loss or vertigo.
In addition to evaluating trauma, CT scans can also aid in the diagnosis and management of other vestibulocochlear nerve disorders. They can identify abnormalities such as congenital malformations or tumors that affect the bony structures. By visualizing these abnormalities, healthcare professionals can determine the most appropriate course of treatment, whether it involves surgical intervention, medication, or other therapeutic approaches.
Overall, both MRI and CT scans play crucial roles in the medical imaging of the vestibulocochlear nerve. While MRI scans excel in visualizing soft tissues and detecting tumors, CT scans provide detailed information about the surrounding bony structures. By combining the information obtained from these imaging techniques, healthcare professionals can make accurate diagnoses and develop effective treatment plans for patients with vestibulocochlear nerve disorders.
Treatment and Management of Vestibulocochlear Nerve Disorders
The vestibulocochlear nerve is a crucial component of the auditory system, responsible for transmitting sound and maintaining balance. When disorders affecting this nerve arise, it is important to explore various treatment and management options to alleviate symptoms and improve overall quality of life.
Surgical Interventions for Vestibulocochlear Nerve Disorders
In cases of vestibular schwannomas or other significant pathologies affecting the vestibulocochlear nerve, surgery may be required. Surgical interventions aim to remove or reduce the tumor’s size and relieve pressure on the nerve. The specific approach and technique depend on the individual case, and it is important to consult with a specialist to determine the most suitable course of action.
One surgical option is microsurgery, which involves using a high-powered microscope and delicate instruments to access and remove the tumor. This technique allows for precise tumor removal while minimizing damage to surrounding structures. Another approach is stereotactic radiosurgery, a non-invasive procedure that delivers targeted radiation to the tumor, causing it to shrink over time.
Recovery from surgery can vary depending on the extent of the procedure and individual factors. Physical therapy and rehabilitation may be necessary to regain balance and improve overall functioning. Regular follow-up appointments with healthcare professionals are essential to monitor progress and address any potential complications.
Non-Surgical Treatments for Vestibulocochlear Nerve Disorders
In some instances, non-surgical treatments may be recommended for vestibulocochlear nerve disorders. These can include monitoring the condition, hearing aids for hearing loss, balance therapy, and medication for symptom management. The choice of treatment depends on the underlying cause, severity of symptoms, and individual patient characteristics. Consulting with a healthcare professional is crucial to develop a personalized treatment plan.
For patients with vestibular schwannomas who are not suitable candidates for surgery, a watch-and-wait approach may be adopted. Regular imaging scans and hearing tests are performed to monitor tumor growth and assess any changes in symptoms. This conservative approach allows for careful observation and intervention if necessary.
Hearing aids can significantly improve auditory function in individuals experiencing hearing loss due to vestibulocochlear nerve disorders. These devices amplify sound and help individuals better understand speech and other sounds in their environment. Balance therapy, on the other hand, focuses on exercises and techniques to improve balance and reduce dizziness or vertigo symptoms.
Medication may also be prescribed to manage symptoms associated with vestibulocochlear nerve disorders. For example, anti-nausea medications can help alleviate dizziness and nausea, while corticosteroids may be used to reduce inflammation and swelling in the nerve.
In conclusion, the vestibulocochlear nerve passes through the cranium via the internal acoustic meatus and plays a vital role in auditory function and balance. Understanding the anatomy, function, and various disorders associated with this nerve is crucial for proper diagnosis and management. Medical imaging techniques, such as MRI and CT scans, aid in visualizing the vestibulocochlear nerve and related pathologies. Treatment options can range from surgical interventions to non-surgical approaches, depending on the specific condition and individual patient needs. Consultation with a medical professional is recommended for accurate diagnosis and personalized treatment planning.