The vestibulocochlear nerve, also known as cranial nerve VIII, plays a crucial role in our auditory and vestibular systems. It is responsible for transmitting sensory information from the inner ear to the brain, allowing us to perceive sound and maintain our balance. Testing for vestibulocochlear nerve function is essential in diagnosing and managing conditions related to this vital nerve.
Understanding the Vestibulocochlear Nerve
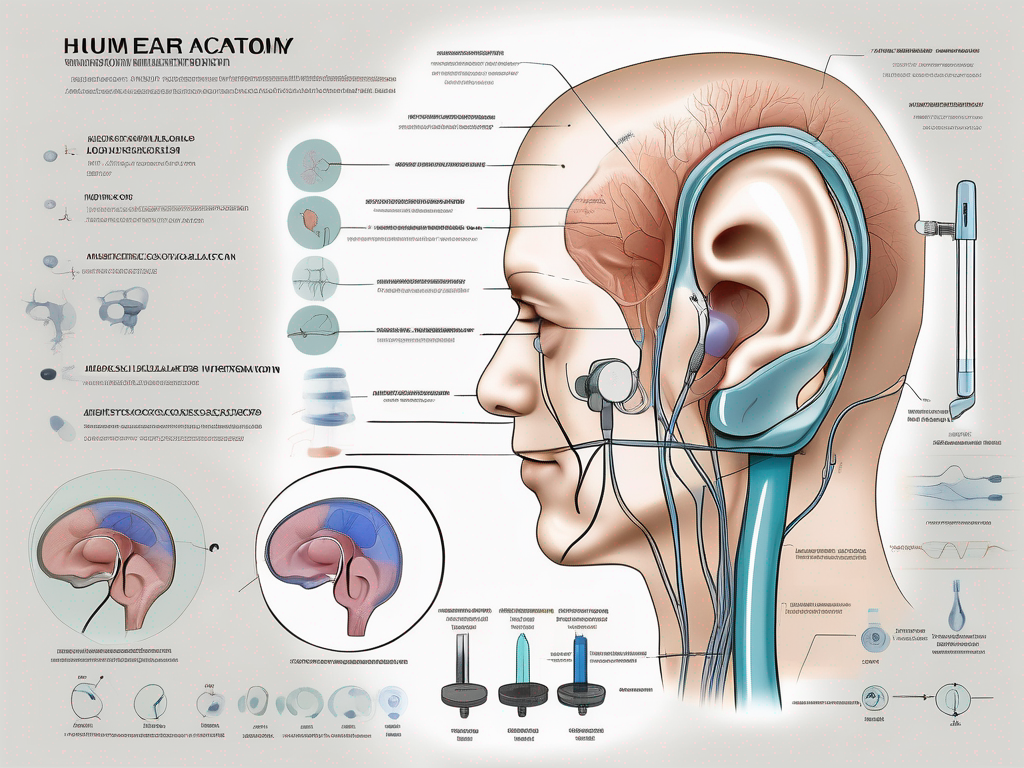
Before delving into the various diagnostic procedures, it is important to have a basic understanding of the anatomy and function of the vestibulocochlear nerve.
The vestibulocochlear nerve, also known as the eighth cranial nerve, plays a crucial role in our ability to hear and maintain balance. It is responsible for transmitting auditory and vestibular signals from the inner ear to various regions of the brain, allowing us to perceive and interpret sounds, as well as maintain our balance and spatial orientation.
Anatomy of the Vestibulocochlear Nerve
The vestibulocochlear nerve is composed of two main divisions: the cochlear nerve and the vestibular nerve.
The cochlear nerve, as the name suggests, is primarily responsible for hearing. It originates from the spiral ganglion located within the cochlea of the inner ear. The cochlea, resembling a snail shell, is a complex structure that converts sound vibrations into electrical signals that can be interpreted by the brain.
The vestibular nerve, on the other hand, governs our sense of balance. It emerges from the vestibular organs, which include the utricle, saccule, and semicircular canals. These organs are filled with fluid and tiny hair cells that detect changes in head position and movement. The vestibular nerve relays this information to the brain, allowing us to maintain our balance and coordinate our movements.
Function of the Vestibulocochlear Nerve
The vestibulocochlear nerve’s primary function is to transmit auditory and vestibular signals from the inner ear to various regions of the brain.
The cochlear portion of the nerve carries sound vibrations to the auditory cortex, a region of the brain responsible for processing sound. Here, the electrical signals generated by the cochlea are decoded and transformed into meaningful auditory information. This intricate process allows us to perceive and interpret sounds, from the softest whispers to the loudest explosions.
The vestibular component of the vestibulocochlear nerve relays information about head movements, helping us maintain balance and spatial orientation. When we move our heads, the fluid in the vestibular organs shifts, stimulating the hair cells and generating electrical signals. These signals are then transmitted through the vestibular nerve to the brain, where they are processed and integrated with visual and proprioceptive information to provide us with a comprehensive perception of our spatial environment.
Without the vestibulocochlear nerve, our ability to hear and maintain balance would be severely compromised. It is a remarkable structure that allows us to navigate the world around us, enjoy the beauty of music, and interact with others through spoken language.
Symptoms of Vestibulocochlear Nerve Damage
Dysfunction or damage to the vestibulocochlear nerve can lead to a range of distressing symptoms. It is important to recognize and understand these symptoms in order to seek appropriate medical attention and treatment.
Hearing Impairment
One of the most common symptoms of vestibulocochlear nerve damage is hearing loss. This can manifest as difficulty hearing certain frequencies, muffled sounds, or a complete loss of hearing in one or both ears. Hearing impairment can have a significant impact on a person’s ability to communicate and engage with the world around them. It can lead to difficulties in social interactions, work, and daily activities.
Furthermore, individuals with vestibulocochlear nerve damage may experience tinnitus, a persistent ringing or buzzing sensation in the ears. This phantom noise can be extremely bothersome and distracting, causing additional distress and discomfort.
Balance Issues
The vestibular component of the vestibulocochlear nerve is essential for maintaining balance and coordinating movements. Damage to this portion can result in various balance issues that significantly affect an individual’s daily life.
Dizziness is a common symptom experienced by those with vestibulocochlear nerve damage. It can range from a mild sensation of lightheadedness to severe vertigo, where the affected person feels as if their surroundings are spinning or moving. Vertigo can be extremely debilitating, making it difficult for individuals to perform even simple tasks.
In addition to dizziness and vertigo, vestibulocochlear nerve damage can cause unsteadiness and problems with coordination. These symptoms make it challenging for individuals to maintain their balance and perform activities that require precise movements, such as walking, climbing stairs, or driving. The fear of falling and the loss of independence that comes with it can greatly impact a person’s quality of life.
It is important to note that the severity and combination of symptoms can vary from person to person, depending on the extent and location of the vestibulocochlear nerve damage. Some individuals may experience only mild hearing impairment or occasional dizziness, while others may face more significant challenges in their daily lives.
If you suspect that you or someone you know may be experiencing symptoms of vestibulocochlear nerve damage, it is crucial to consult with a healthcare professional for a proper diagnosis and appropriate treatment options. Early intervention can help manage the symptoms and improve the overall quality of life for individuals with this condition.
Diagnostic Procedures for Vestibulocochlear Nerve
When evaluating vestibulocochlear nerve function, healthcare professionals employ various diagnostic tests to assess hearing and balance abilities. These procedures are essential in determining the source and extent of nerve damage, guiding appropriate treatment strategies.
The diagnostic procedures for vestibulocochlear nerve involve a range of tests that provide valuable insights into the functioning of the nerve and associated systems. Let’s explore some of these procedures in detail:
Audiometry Test
An audiometry test is a comprehensive assessment of an individual’s hearing abilities. It involves wearing headphones and responding to various tones and words played at different volumes. This test helps determine the range of frequencies a person can hear and identifies any hearing loss or impairment.
During the audiometry test, the healthcare professional presents a series of sounds, ranging from low to high frequencies, to the patient. The patient indicates when they can hear the sound by pressing a button or raising their hand. This test allows the healthcare professional to create an audiogram, a graph that represents the individual’s hearing thresholds at different frequencies.
By analyzing the audiogram, the healthcare professional can identify the type and degree of hearing loss, whether it’s conductive, sensorineural, or mixed. This information is crucial in determining the appropriate treatment options for the patient.
Electronystagmography (ENG)
ENG is a diagnostic procedure used to evaluate the vestibular system’s function and assess eye movements. During this test, electrodes are placed around the eyes to record eye movements while the patient undergoes different head and body positions, as well as exposure to warm or cool air in the ear canals. These measurements aid in identifying abnormalities in the vestibular system.
By monitoring the eye movements, healthcare professionals can assess the functioning of the vestibular system, which is responsible for maintaining balance and spatial orientation. The ENG test helps identify conditions such as vestibular neuritis, Meniere’s disease, and benign paroxysmal positional vertigo (BPPV).
During the ENG test, the patient may be asked to follow a moving target with their eyes or perform specific head movements. The electrodes record the eye movements, which are then analyzed to determine if there are any abnormalities or asymmetries in the vestibular system’s response.
Magnetic Resonance Imaging (MRI)
In some cases, an MRI may be necessary to investigate the cause of vestibulocochlear nerve dysfunction further. This non-invasive imaging technique provides detailed images of the brain and inner ear structures. It can help identify tumors, nerve inflammation, or other structural abnormalities that may be affecting the nerve’s function.
During an MRI, the patient lies on a table that slides into a large, cylindrical machine. The machine uses a powerful magnetic field and radio waves to generate detailed images of the brain and inner ear. These images can reveal any abnormalities that may be causing vestibulocochlear nerve dysfunction.
An MRI is particularly useful in identifying tumors, such as acoustic neuromas, which are noncancerous growths that can affect the vestibulocochlear nerve. It can also help detect other conditions, such as multiple sclerosis or vascular malformations, that may be impacting the nerve’s function.
These diagnostic procedures play a crucial role in evaluating the function of the vestibulocochlear nerve and identifying any underlying conditions or abnormalities. By utilizing a combination of audiometry tests, ENG, and MRI, healthcare professionals can gather comprehensive information to guide treatment decisions and improve patient outcomes.
Interpreting Test Results
After conducting the necessary tests, healthcare professionals analyze the results to make an accurate diagnosis. This crucial step involves carefully examining the data obtained from various diagnostic procedures to gain a comprehensive understanding of the patient’s condition.
One commonly used test is audiometry, which assesses an individual’s hearing abilities. Audiometry results are presented in an audiogram, a graphical representation of the person’s hearing thresholds. A healthcare professional will analyze the audiogram, comparing the person’s hearing thresholds to the normal range. This analysis helps identify the type and degree of hearing loss and informs appropriate treatment options.
Deciphering ENG (Electronystagmography) findings is another important aspect of interpreting test results. ENG results provide information about eye movements associated with different head and body positions and stimuli. A specialist interprets these findings to detect vestibular abnormalities. They carefully analyze the recorded eye movements to determine if there is a vestibulocochlear nerve dysfunction or any other underlying condition affecting the vestibular system.
In addition to audiometry and ENG, healthcare professionals also rely on MRI (Magnetic Resonance Imaging) reports to gain further insights into the patient’s condition. MRI reports are carefully analyzed by radiologists and healthcare professionals trained in diagnostic imaging. They examine the images for any structural abnormalities that could be impacting the vestibulocochlear nerve. These findings help guide further investigations or treatment options.
Interpreting test results is a complex process that requires expertise and attention to detail. Healthcare professionals meticulously analyze the data obtained from various tests to ensure an accurate diagnosis. This comprehensive evaluation helps them develop an appropriate treatment plan tailored to the individual’s unique needs.
Treatment Options for Vestibulocochlear Nerve Damage
Once a diagnosis is confirmed, treatment strategies are tailored to each individual’s specific needs and the underlying cause of the vestibulocochlear nerve damage. It is important to address this condition promptly to prevent further complications and improve quality of life.
When it comes to managing vestibulocochlear nerve dysfunction, there are various treatment options available. These options range from medication and therapy to surgical interventions, depending on the severity of the damage and the symptoms experienced by the individual.
Medication and Therapy
In some cases, medication may be prescribed to manage symptoms related to vestibulocochlear nerve dysfunction, such as vertigo or tinnitus. Medications like antihistamines, antiemetics, or benzodiazepines may be used to alleviate dizziness and nausea associated with vestibular dysfunction. Additionally, corticosteroids may be prescribed to reduce inflammation and promote nerve healing.
Therapies, including vestibular rehabilitation, may also be recommended to help improve balance and mitigate dizziness. Vestibular rehabilitation is a specialized form of physical therapy that focuses on exercises and techniques to strengthen the vestibular system and enhance its ability to compensate for any damage. These exercises may include gaze stabilization, balance training, and habituation exercises to reduce sensitivity to motion.
Furthermore, cognitive-behavioral therapy (CBT) may be utilized to address any psychological distress or anxiety that may arise from the vestibulocochlear nerve damage. CBT can help individuals develop coping mechanisms and strategies to manage the emotional impact of their condition.
Surgical Interventions
In more severe cases, surgical interventions may be considered. These procedures aim to repair or remove any structural abnormalities impacting the vestibulocochlear nerve. The decision to undergo surgery depends on the specific circumstances and the potential benefits outweighing the risks.
One common surgical intervention is the removal of tumors that may be compressing or damaging the vestibulocochlear nerve. This procedure, known as tumor resection, involves the careful removal of the tumor while preserving the surrounding nerves and tissues.
In cases where there is profound hearing loss, cochlear implants may be recommended. Cochlear implants are electronic devices that are surgically implanted into the inner ear to stimulate the auditory nerve directly. This can provide a sense of sound to individuals who have severe or profound hearing loss and are not benefiting from conventional hearing aids.
It is important to note that the decision to undergo surgery should be made in consultation with a healthcare professional who specializes in vestibulocochlear nerve disorders. They will carefully evaluate the individual’s condition, discuss the potential risks and benefits, and provide guidance on the most appropriate course of action.
Overall, the treatment options for vestibulocochlear nerve damage are diverse and aim to address the specific needs of each individual. Whether through medication, therapy, or surgical interventions, the goal is to alleviate symptoms, improve function, and enhance the overall quality of life for those affected by this condition.
Prevention and Maintenance of Vestibulocochlear Health
While not all causes of vestibulocochlear nerve damage are preventable, there are steps individuals can take to maintain the health of their auditory and vestibular systems.
The vestibulocochlear nerve, also known as the eighth cranial nerve, is responsible for transmitting sensory information from the inner ear to the brain. It plays a crucial role in our ability to hear and maintain balance. Damage to this nerve can result in hearing loss, dizziness, and problems with coordination.
Healthy Habits for Ear Health
Protecting the ears from excessive noise exposure is crucial in reducing the risk of hearing loss. Exposure to loud noises, whether it’s from concerts, machinery, or even prolonged use of headphones at high volumes, can cause damage to the delicate structures of the inner ear. To prevent this, it is important to wear ear protection, such as earplugs or earmuffs, in noisy environments. This simple step can significantly reduce the risk of noise-induced hearing loss.
In addition to protecting the ears from loud noises, maintaining proper ear hygiene is essential for vestibulocochlear health. Many people are tempted to clean their ears using cotton swabs, but this can actually do more harm than good. Inserting cotton swabs into the ear canal can push earwax deeper, potentially causing blockages and even damaging the eardrum. Instead, it is recommended to let the ears clean themselves naturally. If excessive earwax becomes a problem, it is best to consult a healthcare professional for safe and effective removal.
Regular Check-ups and Early Detection
Scheduling regular check-ups with a healthcare professional, especially for individuals with a history of ear-related issues or increased risk factors, can aid in early detection and prompt intervention. During these check-ups, healthcare professionals can assess the overall health of the ears and identify any potential problems. Early detection of vestibulocochlear nerve damage allows for timely intervention, which can help prevent further progression of the condition and improve treatment outcomes.
In addition to routine check-ups, it is important to be aware of the signs and symptoms of vestibulocochlear nerve damage. These may include hearing loss, tinnitus (ringing in the ears), vertigo, and difficulty with balance. If any of these symptoms are experienced, it is crucial to seek medical attention promptly. A healthcare professional specializing in ear and vestibular disorders can conduct a thorough evaluation and recommend appropriate treatment options.
In conclusion, testing for vestibulocochlear nerve function plays a crucial role in diagnosing and managing conditions related to the auditory and vestibular systems. Through various diagnostic procedures, healthcare professionals can accurately assess nerve function, guiding appropriate treatment strategies. However, prevention and maintenance of vestibulocochlear health should also be prioritized. By adopting healthy habits, such as wearing ear protection in noisy environments and maintaining proper ear hygiene, individuals can reduce the risk of vestibulocochlear nerve damage. Regular check-ups with healthcare professionals can aid in early detection and intervention, further improving treatment outcomes. If you suspect any issues with your hearing or balance, it is recommended to consult with a healthcare professional, who can provide specialized care and guidance tailored to your individual needs.