The vestibulocochlear nerve, also known as the eighth cranial nerve, plays a crucial role in our ability to hear and maintain balance. Unfortunately, like any other part of our body, it is susceptible to damage and dysfunction. In this article, we will explore the anatomy and function of the vestibulocochlear nerve, common problems that can occur, how to diagnose the damage, available treatment options, and strategies for rehabilitation and prevention.
Understanding the Vestibulocochlear Nerve
The vestibulocochlear nerve, also known as the eighth cranial nerve, is a crucial component of our sensory system. It plays a vital role in our ability to perceive sound and maintain balance. Comprised of two main components, the vestibular nerve and the cochlear nerve, this complex network is responsible for transmitting signals from the inner ear to the brain.
The vestibular nerve, one of the components of the vestibulocochlear nerve, is primarily responsible for relaying information related to balance and spatial orientation. It allows us to navigate our surroundings, ensuring that we maintain an upright posture and move with coordination and grace. Without the vestibular nerve, simple tasks like walking or standing upright would be incredibly challenging.
The cochlear nerve, on the other hand, carries auditory information from the inner ear to the brain. This component of the vestibulocochlear nerve is essential for our ability to hear and interpret sound. It allows us to enjoy the melodies of music, engage in conversations, and appreciate the rich tapestry of sounds that surround us.
Anatomy of the Vestibulocochlear Nerve
The vestibulocochlear nerve originates from the inner ear, specifically the vestibule and cochlea. These structures, nestled deep within the temporal bone, are responsible for converting mechanical vibrations into electrical signals that can be interpreted by the brain. From the inner ear, the vestibulocochlear nerve embarks on a fascinating journey.
Traversing through the internal auditory canal, a narrow passageway within the temporal bone, the vestibulocochlear nerve navigates its way towards the brainstem. Along this intricate pathway, the nerve encounters various structures that play a crucial role in auditory and vestibular processing. These structures include the cochlear nucleus, superior olivary complex, and the inferior colliculus, among others.
Upon reaching the brainstem, the vestibulocochlear nerve establishes connections with these structures, forming a complex network that allows for efficient communication between the ear and the brain. This intricate arrangement ensures that sensory information is relayed accurately and promptly, enabling us to make sense of the world around us.
Function of the Vestibulocochlear Nerve
The primary function of the vestibulocochlear nerve is to relay sensory information from the ear to the brain. When the nerve is functioning optimally, it allows us to maintain balance, perceive sound, and detect changes in our environment. This intricate system ensures that we can navigate our surroundings safely and engage with the auditory world.
When the vestibulocochlear nerve is disrupted or damaged, it can lead to a range of symptoms and complications. Conditions such as vestibular neuritis, Meniere’s disease, and acoustic neuroma can affect the functioning of this nerve, resulting in dizziness, vertigo, hearing loss, and other debilitating symptoms. Understanding the intricate workings of the vestibulocochlear nerve is crucial in diagnosing and treating these conditions effectively.
In conclusion, the vestibulocochlear nerve is a remarkable component of our sensory system. Its intricate anatomy and vital functions allow us to perceive sound, maintain balance, and interact with our environment. By understanding the complexities of this nerve, we can appreciate the wonders of our auditory and vestibular experiences.
Common Vestibulocochlear Nerve Problems
Damage or dysfunction of the vestibulocochlear nerve can have a profound impact on a person’s quality of life. The following sections will explore the symptoms associated with vestibulocochlear nerve damage, as well as the possible causes behind it.
Symptoms of Vestibulocochlear Nerve Damage
When the vestibulocochlear nerve is damaged, individuals may experience a range of symptoms. These include dizziness, vertigo, hearing loss, tinnitus (ringing in the ears), and difficulty maintaining balance. It is important to note that these symptoms can vary in severity and may have different manifestations for each individual.
Dizziness is a common symptom experienced by individuals with vestibulocochlear nerve damage. It is characterized by a sensation of lightheadedness or unsteadiness. People may feel as if the world around them is spinning or moving, leading to a sense of disorientation. This can greatly affect a person’s ability to perform daily activities and can be accompanied by nausea or vomiting.
Vertigo, another symptom associated with vestibulocochlear nerve damage, is a specific type of dizziness. It is characterized by a spinning or whirling sensation, as if the person or their surroundings are rotating. Vertigo can be triggered by certain head movements or can occur spontaneously. It can be extremely debilitating and may last for minutes, hours, or even days.
Hearing loss is a common consequence of vestibulocochlear nerve damage. It can range from mild to severe and can affect one or both ears. Individuals may experience difficulty hearing sounds or understanding speech. This can significantly impact communication and social interactions, leading to feelings of isolation and frustration.
Tinnitus, or ringing in the ears, is another symptom that can accompany vestibulocochlear nerve damage. It is characterized by the perception of sound in the absence of an external source. The sound can be continuous or intermittent and may vary in pitch and intensity. Tinnitus can be a constant distraction and can interfere with concentration and sleep.
Difficulty maintaining balance is a common challenge faced by individuals with vestibulocochlear nerve damage. The vestibular system, which is connected to the vestibulocochlear nerve, plays a crucial role in maintaining balance and spatial orientation. Damage to this system can result in unsteadiness, stumbling, and an increased risk of falls.
Causes of Vestibulocochlear Nerve Damage
Vestibulocochlear nerve damage can occur due to various factors. Trauma, such as head injuries or loud noise exposure, is a common cause. Head injuries, such as those sustained in car accidents or falls, can directly damage the nerve or disrupt its function. Prolonged exposure to loud noises, such as in industrial or concert settings, can also lead to nerve damage over time.
Infections can also contribute to vestibulocochlear nerve damage. Viral infections, such as herpes zoster (shingles) or measles, can affect the nerve and result in inflammation or damage. Bacterial infections, such as meningitis or otitis media, can also lead to nerve damage if left untreated.
Tumors can pose a risk to the vestibulocochlear nerve. Acoustic neuroma, a noncancerous tumor that develops on the nerve responsible for hearing and balance, can cause compression and damage. Other types of tumors, such as meningiomas or schwannomas, can also affect the nerve if they grow in close proximity to it.
Certain medications known to have ototoxic effects can also contribute to vestibulocochlear nerve damage. These include certain antibiotics, chemotherapy drugs, and high doses of aspirin. It is important to be aware of the potential side effects of medications and to discuss any concerns with a healthcare professional.
In conclusion, vestibulocochlear nerve damage can have a significant impact on a person’s well-being. The symptoms can range from dizziness and vertigo to hearing loss and tinnitus. Understanding the causes behind this damage, such as trauma, infections, tumors, or medication side effects, is crucial in order to develop appropriate treatment plans and interventions. If you or someone you know is experiencing symptoms related to vestibulocochlear nerve damage, it is important to seek medical attention for a proper diagnosis and management.
Diagnosing Vestibulocochlear Nerve Damage
Accurately diagnosing vestibulocochlear nerve damage is crucial for effective management. Healthcare professionals employ a combination of medical history assessments, physical examinations, and diagnostic tests to evaluate the integrity of the nerve.
Medical History and Physical Examination
During the medical history assessment, the healthcare provider will inquire about the individual’s symptoms, possible risk factors, and medical background. This information, coupled with a thorough physical examination, can help in identifying potential causes and narrowing down the diagnostic process.
The medical history assessment involves a comprehensive review of the patient’s symptoms. The healthcare provider will ask detailed questions to understand the nature and duration of the symptoms. They will inquire about any associated factors, such as exposure to loud noises, head trauma, or previous ear infections. Additionally, the provider will explore the patient’s medical background, including any pre-existing conditions or medications that could contribute to nerve damage.
After gathering the necessary information from the medical history assessment, the healthcare provider will proceed with a thorough physical examination. This examination focuses on evaluating the patient’s auditory and vestibular systems. The provider will use specialized instruments, such as an otoscope, to examine the ear canal and eardrum for any visible abnormalities. They may also perform tests to assess the patient’s balance and coordination, as these can be affected by vestibulocochlear nerve damage.
Diagnostic Tests for Vestibulocochlear Nerve Damage
Several diagnostic tests are available to evaluate the vestibulocochlear nerve function. Audiometry is commonly used to assess hearing capabilities, while vestibular tests, like electronystagmography, can evaluate the vestibular system’s integrity. Imaging techniques, such as magnetic resonance imaging (MRI), can provide a detailed visual representation of the nerve and surrounding structures.
Audiometry is a non-invasive test that measures the patient’s ability to hear sounds of different frequencies and volumes. It involves wearing headphones and responding to various tones or words. This test helps determine the extent and type of hearing loss, which can indicate vestibulocochlear nerve damage.
Vestibular tests, like electronystagmography, assess the function of the vestibular system, which is responsible for maintaining balance and spatial orientation. During this test, the patient may be asked to follow moving objects with their eyes or undergo positional changes to provoke dizziness or nystagmus (involuntary eye movements). These tests can help identify any abnormalities in the vestibulocochlear nerve or other structures involved in balance regulation.
In some cases, healthcare providers may recommend imaging techniques, such as magnetic resonance imaging (MRI), to obtain detailed images of the vestibulocochlear nerve and surrounding structures. MRI uses powerful magnets and radio waves to create high-resolution images, allowing healthcare professionals to visualize any structural abnormalities or damage to the nerve.
Overall, the combination of medical history assessments, physical examinations, and diagnostic tests plays a crucial role in accurately diagnosing vestibulocochlear nerve damage. These comprehensive evaluations help healthcare professionals develop an effective management plan tailored to the individual’s specific needs.
Treatment Options for Vestibulocochlear Nerve Damage
When it comes to managing vestibulocochlear nerve damage, there are various treatment options available that aim to alleviate symptoms and improve functional outcomes. These treatment options can be categorized into non-surgical and surgical interventions, depending on the underlying cause and severity of the condition.
Non-Surgical Treatments
Non-surgical approaches for vestibulocochlear nerve damage primarily focus on symptom management and lifestyle modifications. Medication management plays a crucial role in alleviating symptoms associated with nerve damage. Healthcare professionals may prescribe corticosteroids or anti-vertigo drugs to reduce inflammation and dizziness, respectively. These medications can provide relief and improve the overall quality of life for individuals with vestibulocochlear nerve damage.
In addition to medication, lifestyle modifications can also have a significant impact on managing symptoms. Avoiding loud noises and environments that may exacerbate symptoms is crucial. Noise-induced hearing loss can further damage the already compromised vestibulocochlear nerve, so taking steps to protect the ears is essential. Furthermore, stress-reducing techniques, such as meditation or relaxation exercises, can help minimize the impact of stress on symptoms.
For individuals experiencing hearing loss due to vestibulocochlear nerve damage, hearing aids can be a valuable tool. These devices amplify sound and improve the ability to hear, enhancing communication and overall quality of life. Additionally, balance therapy exercises may be recommended to improve stability and reduce dizziness. These exercises are designed to strengthen the body’s balance system, helping individuals regain confidence in their ability to move and navigate their surroundings.
Surgical Treatments
In certain cases, surgical intervention may be necessary to address vestibulocochlear nerve damage. The decision to pursue surgery should be made in consultation with a qualified healthcare professional, who will carefully consider the potential risks and benefits associated with the specific case.
One possible surgical procedure involves the removal of tumors that may be compressing or damaging the vestibulocochlear nerve. These tumors, such as acoustic neuromas or meningiomas, can cause significant impairment and require surgical intervention to alleviate symptoms and prevent further damage.
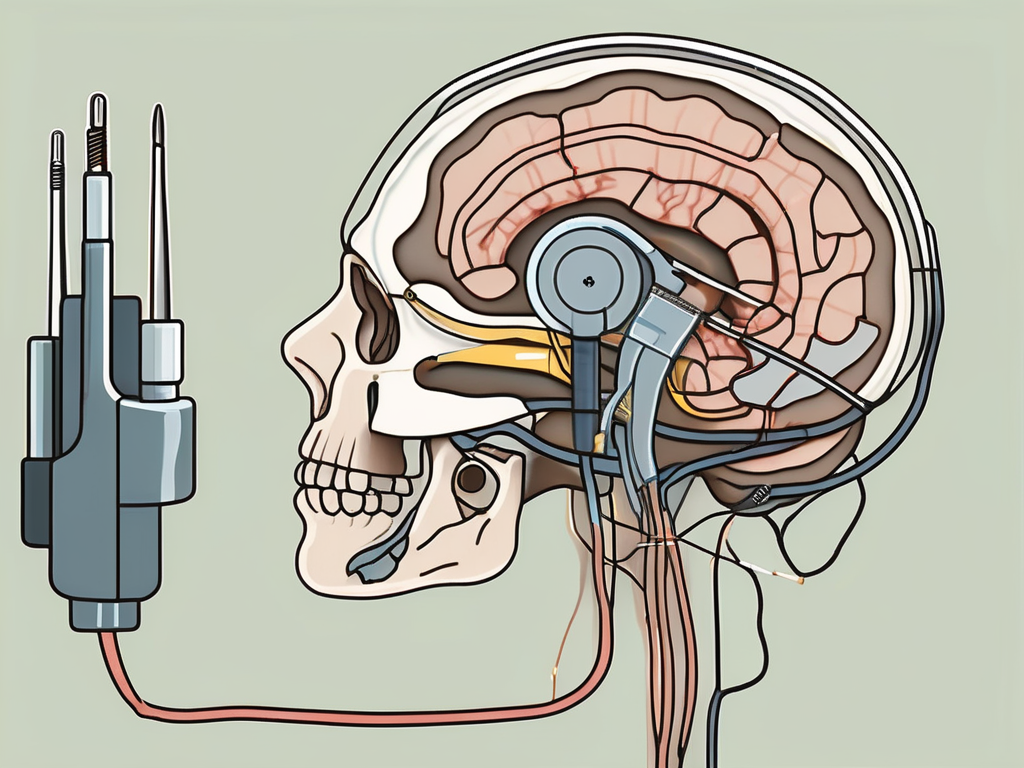
In some instances, structural abnormalities within the ear may contribute to vestibulocochlear nerve damage. Surgical procedures can be performed to repair these abnormalities, aiming to restore normal function and alleviate symptoms. These procedures may involve reconstructing the middle ear or repairing the cochlea, depending on the specific issue at hand.
For individuals with severe hearing loss, cochlear implantation may be considered. Cochlear implants are electronic devices that bypass the damaged parts of the inner ear and directly stimulate the auditory nerve, allowing individuals to perceive sound. This surgical intervention can significantly improve hearing abilities and enhance communication skills.
It is important to note that the appropriateness of surgical treatments for vestibulocochlear nerve damage varies on a case-by-case basis. A thorough evaluation by a qualified healthcare professional is necessary to determine the most suitable treatment approach.
Rehabilitation and Recovery from Vestibulocochlear Nerve Damage
Recovering from vestibulocochlear nerve damage often requires a comprehensive rehabilitation program. Physical therapy can play a crucial role in improving balance, coordination, and mobility. A skilled therapist will develop an individualized treatment plan to address specific impairments and help restore optimal function. Additionally, coping strategies and support groups can provide emotional and psychological assistance for individuals navigating the challenges associated with vestibulocochlear nerve damage.
Physical Therapy for Vestibulocochlear Nerve Damage
Physical therapy for vestibulocochlear nerve damage typically involves exercises and techniques aimed at improving balance, coordination, and gait. Therapists may employ various methods, such as vestibular rehabilitation exercises, gaze stabilization training, and proprioceptive training. Regular sessions, guided by a qualified therapist, can gradually restore functionality and enhance overall quality of life.
Coping Strategies and Support for Patients
Dealing with vestibulocochlear nerve damage can be challenging, both emotionally and physically. It is important for individuals to seek support from healthcare professionals, such as counselors or psychologists, who can provide guidance and coping strategies. Support groups and online forums may also offer a valuable network of individuals facing similar experiences, fostering a sense of community and understanding.
Prevention of Vestibulocochlear Nerve Damage
While some causes of vestibulocochlear nerve damage are unavoidable, there are proactive measures that individuals can take to minimize the risk of injury or deterioration.
Lifestyle Changes to Prevent Damage
Protecting the vestibulocochlear nerve can be achieved through simple lifestyle modifications. Avoiding exposure to excessive noise, wearing ear protection in noisy environments, and adopting healthy habits, such as regular exercise and a balanced diet, can positively influence overall nerve health. Regular check-ups with an audiologist or otolaryngologist are also recommended to detect any potential issues early on.
Regular Check-ups and Early Detection
Regular check-ups with healthcare professionals trained in auditory and vestibular assessments are crucial for early detection of any potential issues. Prompt identification allows for timely intervention, which can prevent further damage and assist in achieving better outcomes. Individual monitoring and self-awareness of any changes in hearing or balance should also be prioritized.
In conclusion, the vestibulocochlear nerve plays an indispensable role in our auditory and vestibular functions. Damage or dysfunction of this nerve can lead to various symptoms and impairments. However, with proper diagnosis, appropriate treatment options, and comprehensive rehabilitation, individuals can effectively manage their conditions. Remember, if you suspect any issues with your vestibulocochlear nerve, consult with a healthcare professional experienced in treating auditory and vestibular disorders for guidance tailored to your specific needs.