The auditory function of the vestibulocochlear nerve is essential for proper hearing and balance. Dysfunction or damage to this nerve can result in various auditory and vestibular disorders. Fortunately, there are several tests available to assess the auditory function of the vestibulocochlear nerve accurately. In this article, we will delve into the anatomy of the vestibulocochlear nerve, explain the basics of auditory function testing, explore specific tests for the vestibulocochlear nerve, discuss the interpretation of test results, examine the treatment and management of vestibulocochlear nerve disorders, and look at the future directions in auditory function testing.
Understanding the Vestibulocochlear Nerve
The vestibulocochlear nerve, also known as Cranial Nerve VIII, consists of two main components: the vestibular nerve, responsible for balance and spatial orientation, and the cochlear nerve, responsible for auditory perception. These two nerves work harmoniously to provide us with a sense of equilibrium and allow us to perceive sound. Understanding the anatomy and role of the vestibulocochlear nerve is crucial to comprehending how auditory function testing is carried out.
Anatomy of the Vestibulocochlear Nerve
The vestibulocochlear nerve originates from the inner ear and extends towards the brainstem, where it connects with the vestibular and cochlear nuclei. The vestibular nerve comprises a series of intricate structures called the semicircular canals, responsible for detecting rotational movements, and the otolith organs, responsible for detecting linear acceleration and changes in head position. These structures are filled with fluid and contain tiny hair cells that convert mechanical movement into electrical signals, which are then transmitted through the vestibulocochlear nerve.
The semicircular canals, three in each ear, are arranged perpendicular to each other and are responsible for detecting movements in different planes. When we rotate our head, the fluid in these canals moves, stimulating the hair cells and sending signals to the brain about the direction and speed of the movement. This information is crucial for maintaining balance and coordinating eye movements.
The otolith organs, consisting of the utricle and saccule, are responsible for detecting linear acceleration and changes in head position. They contain tiny calcium carbonate crystals called otoliths, which are attached to hair cells. When we move in a straight line or change our head position, the otoliths shift, bending the hair cells and generating electrical signals that are transmitted through the vestibulocochlear nerve. This information helps us maintain a stable posture and perceive changes in our orientation with respect to gravity.
On the other hand, the cochlear nerve is responsible for transmitting sound signals from the cochlea, a spiral-shaped organ in the inner ear, to the brain for auditory processing. The cochlea is divided into three fluid-filled compartments, and it contains the organ of Corti, which is the main structure responsible for converting sound vibrations into electrical signals. The organ of Corti contains thousands of hair cells that are arranged in rows and are responsible for detecting different frequencies of sound. When sound waves enter the cochlea, they cause the fluid to move, which in turn stimulates the hair cells. These hair cells convert the mechanical energy of the sound waves into electrical signals, which are then transmitted through the cochlear nerve to the brain for further processing.
Role in Auditory Function
The vestibulocochlear nerve plays a vital role in auditory function by carrying auditory signals from the cochlea to the auditory cortex in the brain. It allows us to perceive and interpret sounds, including speech, music, and environmental noises. The auditory cortex is responsible for processing these signals and giving meaning to the sounds we hear. Different regions of the auditory cortex are specialized for processing different aspects of sound, such as pitch, rhythm, and timbre.
Damage or dysfunction to the vestibulocochlear nerve can result in hearing loss or tinnitus, affecting an individual’s quality of life. Hearing loss can be conductive, sensorineural, or mixed, depending on the location and nature of the damage. Conductive hearing loss occurs when there is a problem with the transmission of sound waves from the outer or middle ear to the inner ear. Sensorineural hearing loss, on the other hand, occurs when there is damage to the hair cells in the cochlea or the auditory nerve. Mixed hearing loss is a combination of conductive and sensorineural hearing loss.
A variety of factors can cause damage to the vestibulocochlear nerve, including exposure to loud noises, certain medications, infections, tumors, and aging. It is important to protect our ears from excessive noise and seek medical attention if we experience any changes in our hearing or balance. Audiologists and otolaryngologists are healthcare professionals who specialize in diagnosing and treating disorders of the vestibulocochlear nerve and the auditory system as a whole.
Basics of Auditory Function Testing
When it comes to assessing the auditory function of the vestibulocochlear nerve, various tests are available. These tests aim to evaluate an individual’s ability to detect and interpret sound accurately. Regular auditory function testing is essential for early detection of any auditory abnormalities, as prompt intervention can make a significant difference in the outcome.
Importance of Auditory Testing
Testing the auditory function of the vestibulocochlear nerve is crucial not only for diagnosing hearing loss or balance disorders but also for monitoring the effectiveness of any treatment or intervention. By conducting auditory tests, healthcare professionals can gather valuable information about an individual’s hearing thresholds, speech recognition abilities, and the overall health of the auditory system.
Regular auditory testing is especially important for individuals who are at a higher risk of developing hearing loss, such as those with a family history of hearing impairment, individuals who work in noisy environments, or those who have been exposed to loud noises for an extended period.
Moreover, auditory testing is also essential for children, as early detection of hearing loss can significantly impact their speech and language development. By identifying any hearing difficulties at an early stage, appropriate interventions can be implemented to ensure optimal communication skills and overall cognitive development.
General Procedure of Auditory Tests
The general procedure of auditory tests involves a series of assessments that measure an individual’s hearing sensitivity, speech perception, and middle ear function. These tests are non-invasive and typically painless.
First, an audiologist will conduct a thorough case history, including questions about any previous ear infections, trauma, or exposure to loud noise. They will also inquire about any symptoms and assess the impact of hearing loss on an individual’s daily life.
During the case history, the audiologist may also ask about any medications the individual is taking, as certain medications can have ototoxic effects, potentially causing damage to the auditory system.
Next, the audiologist will perform a physical examination of the ears, checking for any visible abnormalities or blockages. This examination allows them to rule out any external factors that may be affecting the auditory function.
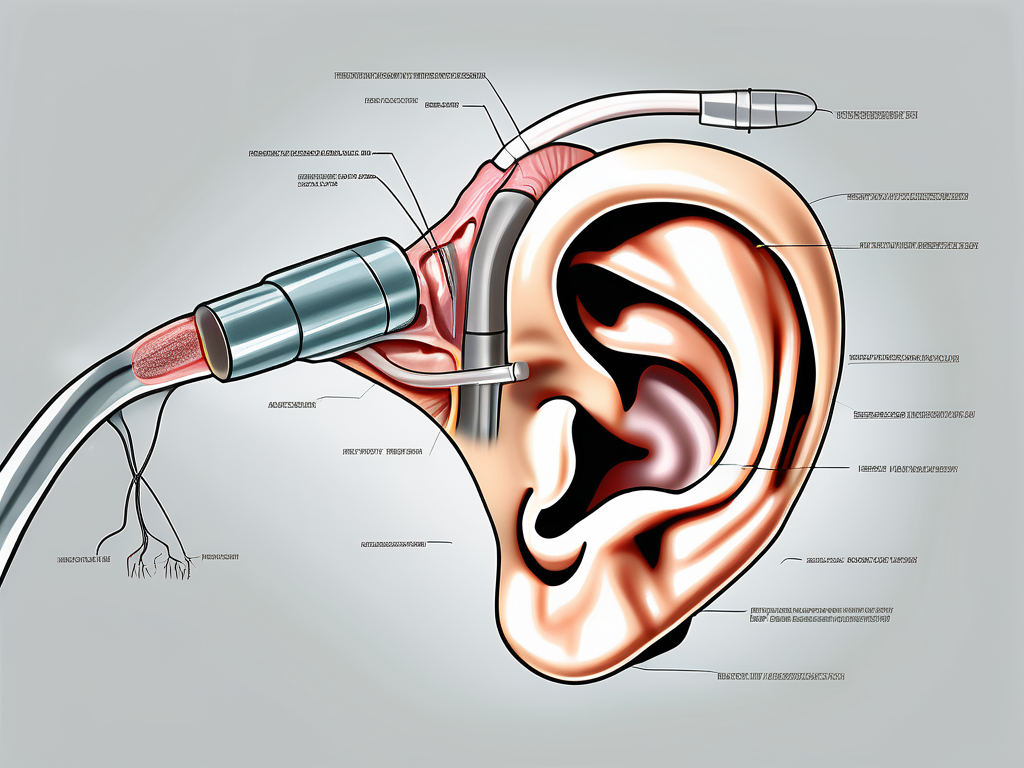
During the physical examination, the audiologist may use an otoscope to examine the ear canal and the eardrum. They will also assess the mobility of the eardrum by performing a test called tympanometry. Tympanometry measures the movement of the eardrum in response to changes in air pressure, providing information about the middle ear function.
Following the physical examination, the audiologist will proceed with a battery of tests to evaluate different aspects of auditory function. These tests may include pure-tone audiometry, speech audiometry, tympanometry, and auditory brainstem response (ABR) test, among others.
Pure-tone audiometry is the most common test used to assess an individual’s hearing thresholds. During this test, the individual wears headphones and listens to a series of tones at different frequencies and volumes. They are then asked to indicate when they can hear each tone, allowing the audiologist to determine the softest sounds the individual can detect at different frequencies.
Speech audiometry, on the other hand, evaluates an individual’s ability to understand and repeat spoken words. This test helps determine the individual’s speech recognition abilities and provides insight into how well they can understand speech in various listening conditions.
In addition to these tests, the audiologist may also perform an auditory brainstem response (ABR) test. This test measures the electrical activity of the auditory nerve and brainstem in response to sound stimuli. It can help identify any abnormalities in the auditory pathway and provide information about the integrity of the auditory system.
Overall, auditory function testing plays a crucial role in assessing an individual’s hearing abilities and identifying any auditory abnormalities. By conducting a comprehensive battery of tests, healthcare professionals can gather valuable information to guide appropriate interventions and ensure optimal auditory health.
Specific Tests for the Vestibulocochlear Nerve
To specifically assess the auditory function associated with the vestibulocochlear nerve, several tests can provide valuable insights. These tests not only help diagnose hearing disorders but also aid in understanding the underlying mechanisms of auditory perception.
Pure-Tone Audiometry
Pure-tone audiometry is one of the most commonly used tests to measure an individual’s hearing thresholds. During this test, the audiologist presents a range of tones at different frequencies and volumes. The individual must indicate when they hear each tone, allowing the audiologist to determine the softest sounds they can detect at various frequencies.
This test provides a comprehensive evaluation of an individual’s hearing abilities across different frequencies. By plotting the results on an audiogram, the audiologist can identify the type and degree of hearing loss, if present. Pure-tone audiometry is crucial in determining the appropriate treatment options, such as hearing aids or cochlear implants, for individuals with hearing impairments.
Speech Audiometry
Speech audiometry assesses an individual’s ability to perceive and understand speech. The audiologist may use various speech stimuli, such as phonetically balanced words or sentences, to evaluate speech recognition abilities accurately. This test provides valuable information about an individual’s ability to comprehend speech in different listening conditions.
By measuring the individual’s speech reception threshold (SRT) and word recognition score (WRS), the audiologist can determine the level at which speech becomes audible and the percentage of words correctly understood. This information helps in diagnosing and managing communication difficulties caused by auditory processing disorders or hearing loss.
Tympanometry
Tympanometry is a test that evaluates the movement of the eardrum and middle ear by applying air pressure changes to the ear canal. It helps identify any abnormalities in the middle ear, such as fluid accumulation or eardrum stiffness, which may affect auditory function.
During the test, a probe is inserted into the ear canal, and air pressure variations are introduced. By measuring the compliance of the eardrum and the impedance of the middle ear, the audiologist can assess the condition of the middle ear and identify potential causes of conductive hearing loss. Tympanometry is particularly useful in diagnosing conditions like otitis media, tympanic membrane perforations, or Eustachian tube dysfunction.
Auditory Brainstem Response (ABR) Test
The auditory brainstem response test measures the electrical activity of the auditory nerve and specific brainstem structures in response to sound stimuli. Electrodes are placed on the individual’s scalp to record the responses, which provide insights into the integrity and function of the vestibulocochlear nerve.
This test is commonly used for newborn hearing screening and assessing individuals with suspected auditory neuropathy or retrocochlear disorders. By analyzing the waveform patterns generated by the auditory system, the audiologist can determine the presence of any abnormalities or delays in the transmission of auditory signals along the auditory pathway.
The ABR test is particularly valuable in diagnosing conditions like acoustic neuroma, multiple sclerosis, or brainstem lesions that may affect the vestibulocochlear nerve. It helps guide further diagnostic investigations and treatment planning.
Interpreting Test Results
Interpreting the results of auditory function tests requires expertise and experience. Audiologists analyze the data collected during the tests to determine the individual’s hearing thresholds, speech recognition abilities, and the overall health of the auditory system. One of the key tools used for interpretation is an audiogram.
When it comes to understanding auditory function tests, there is a wealth of information that can be gleaned from the data collected. Audiologists carefully examine the results to identify any abnormalities or patterns that may indicate potential issues with the individual’s hearing. By analyzing the audiogram, which is a graph representing an individual’s hearing thresholds at different frequencies, audiologists can gain valuable insights into the type, degree, and configuration of hearing loss.
Understanding Audiograms
An audiogram is a graph that represents an individual’s hearing thresholds at different frequencies. It helps visualize the type, degree, and configuration of hearing loss. By comparing an individual’s audiogram to normal hearing ranges, audiologists can identify potential issues in the vestibulocochlear nerve and recommend appropriate interventions or treatments.
When examining an audiogram, audiologists pay close attention to the shape of the graph. Different shapes can indicate different types of hearing loss. For example, a sloping audiogram suggests high-frequency hearing loss, while a flat audiogram may indicate a more evenly distributed hearing loss across all frequencies. These subtle nuances in the audiogram can provide valuable clues about the underlying condition affecting the individual’s auditory system.
In addition to the shape of the audiogram, the specific thresholds at different frequencies are also crucial in interpreting the test results. By comparing the individual’s thresholds to the normal hearing ranges, audiologists can determine the severity of the hearing loss. This information is vital in developing an appropriate treatment plan tailored to the individual’s specific needs.
Indications of Vestibulocochlear Nerve Damage
Abnormalities in the test results, such as elevated hearing thresholds or decreased speech recognition scores, may suggest damage or dysfunction of the vestibulocochlear nerve. These indications require further investigation and may warrant referral to an otolaryngologist or a neurologist for additional evaluation and treatment options.
When interpreting test results, audiologists consider a range of factors beyond just the audiogram. They take into account the individual’s medical history, any symptoms they may be experiencing, and the results of other tests, such as speech recognition tests or middle ear assessments. By combining all of this information, audiologists can form a comprehensive understanding of the individual’s auditory health and make informed recommendations for further evaluation or treatment.
It’s important to note that interpreting test results is not a one-size-fits-all process. Each individual is unique, and their test results should be interpreted in the context of their specific circumstances. This personalized approach ensures that the individual receives the most accurate diagnosis and appropriate care for their auditory needs.
Treatment and Management of Vestibulocochlear Nerve Disorders
While treatment options for vestibulocochlear nerve disorders depend on the specific diagnosis, there are various therapeutic approaches and lifestyle adjustments that can benefit individuals with auditory dysfunction.
Therapeutic Approaches
Treatment options range from conservative approaches, such as hearing aids or assistive listening devices, to more invasive interventions, such as cochlear implants or surgical procedures. The choice of treatment depends on the individual’s specific condition, the severity of the auditory dysfunction, and their personal preferences.
Lifestyle Adjustments for Improved Auditory Health
In addition to medical interventions, making certain lifestyle adjustments can help improve auditory health. These adjustments include protecting the ears from loud noise, adopting healthy habits, such as regular exercise and a balanced diet, and managing stress levels, which can indirectly impact auditory function.
Future Directions in Auditory Function Testing
The field of auditory function testing is continuously evolving, with ongoing research and technological advancements opening up new possibilities for more accurate diagnoses and tailored interventions.
Advances in Auditory Testing Technology
Advances in technology, such as the development of portable and more precise audiometric devices, have revolutionized auditory testing. These advancements allow for greater accessibility and accuracy in diagnosing auditory disorders, benefiting both healthcare professionals and individuals seeking auditory evaluation.
Emerging Research in Auditory Health
Ongoing research in the field of auditory health aims to improve our understanding of the vestibulocochlear nerve and its connection to various auditory disorders. This research may lead to new treatment modalities, preventive strategies, and a more comprehensive approach to managing vestibulocochlear nerve-related conditions.
In conclusion, testing the auditory function of the vestibulocochlear nerve is crucial for diagnosing and managing various auditory and balance disorders. Through a series of tests, healthcare professionals can accurately evaluate an individual’s auditory function and customize interventions accordingly. It is important for individuals experiencing any signs of hearing loss or balance issues to consult with an audiologist or healthcare provider to receive appropriate evaluation and guidance. By staying informed and proactive about auditory health, individuals can access the necessary support and enjoy an improved quality of life.